In observance of Cancer Immunotherapy Month in June, we have invited guest contributor Shawn Tallet, Outreach Coordinator for the Mesothelioma & Asbestos Awareness (MAA) Center to offer a brief look at immunotherapy, its history and promise as a treatment. We are particularly excited about the possibility of immunotherapy for use in pediatric cancer, and happy to share the following update.
Tremendous strides have been made in the field of oncological research and treatment, but perhaps the most sustainable and discernable advancements fall within the realm of immunotherapy. Broadly speaking, immunotherapy is the use of the body’s own immune system to combat and eradicate cancerous cells. Today, several different types of immunotherapy are used in treating the disease, including cancer vaccines and antigen therapy. The success rate has been climbing substantially, and certain treatment regimens have been effective in combating pediatric cancer and other rare diseases, as well as providing patients a less toxic therapy option.
Early Beginnings
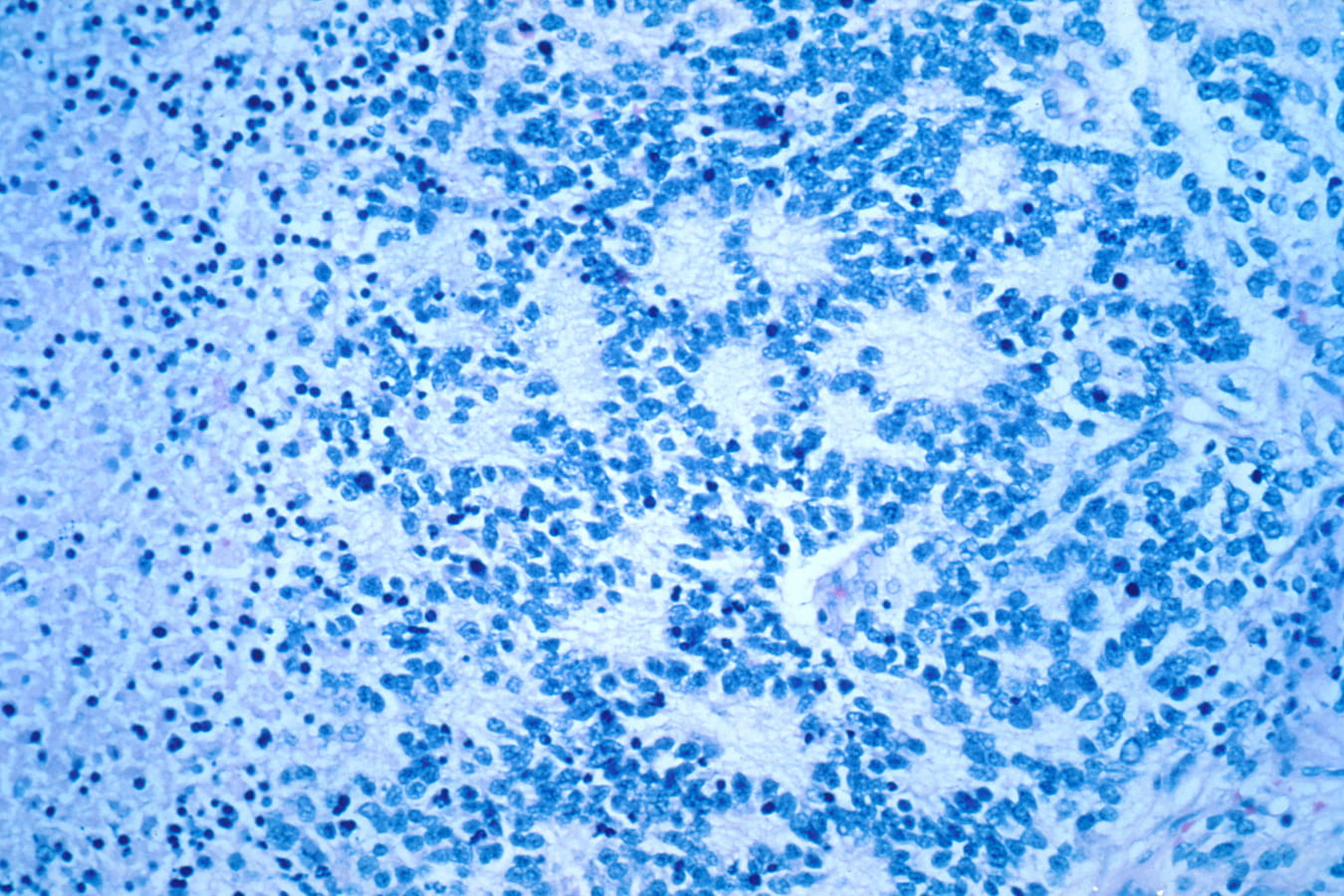
Although immunotherapy can be traced back to the late 19th century, its practical application and understanding wasn’t fully integrated into cancer care until the 1990s. Dr. William B. Coley, MD, is generally considered the first practitioner who championed immunotherapy in the late 1800s. Dr. Coley’s theory that live and inactivated antigens injected directly into tumors would elicit an immune response was accurate, and some patients with sarcomas, lymphoma, and testicular carcinoma went into spontaneous remission. This strategy was continually extrapolated upon throughout the 20th century, resulting in a major breakthrough in 1976. Researchers were able to pinpoint T-cell growth factors and understand their interaction with cancer cells. Antibody therapy regimens and cancer vaccines were eventually discovered and offered in clinical trials, with the first Food and Drug Administration (FDA) approval occurring in 2010. These vaccines were shown to extend overall survival rates in clinical trials, and many childhood cancers have been included in these experimental treatments, including non-Hodgkin lymphoma, neuroblastoma, and several types of leukemia.
Modern Therapy
There are many variables associated with the decision to start immunotherapy, and they should be thoroughly discussed with one’s oncologist. Since many types of immunotherapy are still in experimental phases, they are not always approved by the FDA. However, because immunotherapy uses the body’s own defense system to fight disease, side-effects are generally more mild than regimens like chemotherapy and radiation therapy which use toxins to destroy cancer cells. Certain pediatric cancers have seen great success in treatment with monoclonal antibody therapies, most notably relapsed B-cell acute lymphoblastic leukemia (ALL), which is treated with FDA-approved KYMRIAH, a therapy specially designed for patients under 25 years of age. Furthermore, vaccination clinical trials targeting neuroblastoma, as well as sarcomas in infants and young children, can be successful. Additionally, some rare diseases have shown positive responses to immunotherapy treatments. Patients with mesothelioma, a rare disease caused by asbestos exposure, have had success with immunotherapy treatments used for non-small cell lung cancer. Under the right circumstances, including overall patient health and stage of cancer, these treatment procedures have resulted in the reduction of cancerous growth and even near complete remission.
What Does the Future Hold?
With the rate of medical research and advancement occurring throughout the world, the sense of optimism in cancer treatment is at an all-time high. Immunotherapy is perhaps the most cutting-edge mode of treatment in development and moves away from types of treatments with known toxicities to patients, like chemo and radiation therapy. In the past two years incredible progress has been made in the field, with milestones including gene editing to prompt immune cells to fight cancer (University College London, April 2016) and FDA approvals of CAR-T therapies (University of Pennsylvania, August 2017).
This extensive study of the immune system’s potential moves the world one step closer to finding the ultimate cure to end cancer.
For more information on immunotherapy and the MAA Center, visit www.maacenter.org/treatment/emerging-treatments

Recent Comments